Led by the Bone and Joint Research Group at the University of Southampton, the research resulted in the first custom-made hip replacement using stem cells, plus the formation of a University of Southampton spin-out, Renovos Biologics Limited (Renovos).
This orthopaedic biologic company is developing a novel nanoclay, RENOVITE®, that provides a platform technology for medical applications, including orthopaedics, wound repair and dental.
Renovos has raised £870,000 in private and public sector funding between 2017 and 2020. In 2023, Renovos began a significant partnership with Biocomposites.
This work has been led by:
- Professor Richard Oreffo, Professor of Musculoskeletal Science and Chief Scientific Officer for Renovos
- Professor Jonathan Dawson, EPSRC Research Fellow and Chief Technology Officer for Renovos
Both professors are based at the University of Southampton and co-founded Renovos with Dr Agnieszka Janeczek, Chief Executive Officer of Renovos, and Mr James Otter, Chair.
The development of the technology behind these impacts has been backed by more than 20 project grants led by Professor Oreffo, totalling £8.4 million, and several more awards where he has been a co-investigator. This investment has been truly multidisciplinary, involving grants mostly from the Biotechnology and Biological Sciences Research Council (BBSRC), along with the Medical Research Council (MRC) and the Engineering and Physical Sciences Research Council (EPSRC). Innovate UK has also awarded a further £1.1 million for research led by Renovos, post-spin-out, for further development of RENOVITE®.
This long-term and multidisciplinary funding, spread over more than 20 years, has been crucial in underpinning Professor Oreffo’s and Professor Dawson’s research and its exciting outcomes.
Fragility fractures
In 2018, the National Institute for Health and Care Excellence reported that, annually, there are over 500,000 fragility fractures associated with osteoporosis in the UK, costing around £4.4 billion. Hip fractures alone cost the NHS £2 billion. Around 24% of hip fractures are treated with a total hip replacement but still pose significant challenges for patients and the NHS. Individually, primary hip replacements cost the NHS around £6,000, with revisions at £18,000. Around 20% of primary hip replacements are replaced in 10 years, and these surgeries carry much higher risks of infections and complications.
The impact these injuries have on movement and function also affects the economy, in terms of the UK workforce and spending ability.
Furthermore, the International Osteoporosis Foundation estimates that, internationally, around 20% of individuals will die within the first year after a hip fracture. These injuries also take a massive toll on the mental and physical welfare of patients and cause serious and sometimes long-term pain.
Combining hip replacements with tissue engineering could improve the longevity of replacements, improve patient outcomes and decrease economic pressure.
What are stem cells?
Stem cells can grow, repair and regenerate, helping us heal tissues that are damaged through injury, disease or normal wear and tear. This also makes them useful for medical or research applications, including bone marrow transplants and generating cell lines for research.
Skeletal adult stem cells are found in bone marrow and can form fat, cartilage and bone under the right conditions. When taken from a patient, skeletal stem cells can be used for personalised medicine and are far less likely to trigger rejection. Stem cells need the right environment to thrive, including:
- something to adhere to for growth, like a scaffold
- the right signals (biochemical molecules) to activate them
- a good supply of blood and oxygen for successful tissue growth
Decades of research have gone into engineering the perfect microenvironment for skeletal stem cell growth, including several projects led by Professor Oreffo. We are now at the point where stem cells are being used in humans to treat bone damage and related injuries. Funding from UK Research and Innovation (UKRI) councils has enabled the groundwork needed to test, commercialise and utilise the technologies for healthcare.
Interdisciplinary and multi-council investment for success
In 2002, funding from BBSRC, EPSRC, the Nuffield Foundation and DePuy International Ltd led to Professor Oreffo’s discovery that skeletal stem cells could be isolated from humans and used to form new bone. When combined with polylactic acid scaffolds (3D-printable biodegradable material that supports tissue formation) and implanted into mice, new bone was formed.
BBSRC, EPSRC and MRC funding dovetailed to enable research and the development of technologies, including:
- collaboration with the Southampton General Hospital to study cell samples from human femurs and to develop new approaches for their growth
- generating new tissue and treating femur-related conditions by combining a patient’s own skeletal stem cells with donated bone tissue to make a graft
- developing new scaffold materials and approaches for supporting bone stem cell growth and repair
A world-first hip surgery
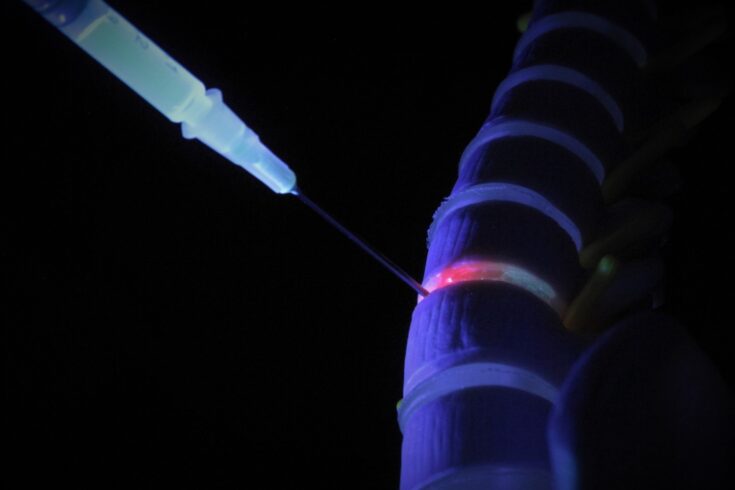
In 2014, this long-term funding resulted in the first-ever hip surgery with a 3D custom-made hip replacement and bone stem cell graft, performed at Southampton General Hospital. The hip implant is made from titanium and designed using a CT scan and ‘computer aided design and computer aided manufacturing’ (CAD CAM) technology for exact measurements. The patient’s bone marrow cells are extracted and used to regenerate bone around the implant, fusing the material and bone together.
The first recipient was a 71-year-old whose hip had been crushed in a car accident 37 years prior. Six years later, the patient remained mobile and free of pain. Between 2014 and 2020 (pre-COVID-19), a further 20 patients were treated using this method. Many of these patients had significant bone loss due to previous failed replacements and some were immobile or used a wheelchair. A 2020 review showed that no replacements were needed, and there had been no further dislocations or fractures.
The 2021 Research Excellence Framework (REF) impact case study on Professor Oreffo’s research emphasised that this method could save the NHS a significant amount of money through reduced need for revisions and improved quality of life. It was estimated that, assuming a best-case scenario of 50% implant survival enhancement for all 3,150 annual patients, these hip replacements would save the NHS £34.8 million.
Delivering molecules for bone repair
Professor Oreffo worked with Professor Dawson on novel biomaterials for bone repair. They were amongst the first to use nanoclay gels in this area of research. Clay nanoparticles are a great delivery agent due to their ability to stick together to form gels that localise and stabilise biomolecules.
Professor Dawson began working on the topic during his BBSRC-funded Strategic Research Studentship PhD into how Laponite, a clay gel, could deliver bone stem cells for repairing injuries. He is now an EPSRC-funded fellow and is the current Director of the Centre for Human Development, Stem Cells and Regeneration.
This research has produced clay gels that stay localised to injury sites and form scaffolds that deliver stem cells, support tissue growth, and coordinate molecules. They focused on bone morphogenic protein 2 (BMP-2), a protein that strongly stimulates bone growth, which is currently used clinically for fusing bones in difficult cases. However, it requires high doses and risks dangerous side effects.
Dawson and Oreffo’s clay gel binds strongly to BMP-2, keeping it highly localised and dramatically reducing the dosage needed, which could improve the safety of BMP-2 usage in patients. Professor Dawson’s EPSRC fellowship funding was the major support for this clay nanogel research, including developing the clay gel and proving the nanoclay could form new bone material in vitro with a safe BMP-2 dose.
In 2017, Professor Dawson and Professor Oreffo founded the spin-out Renovos to commercialise the technology, together with Dr Janeczek (a former research student) and Mr Otter.
Renovos is establishing the manufacture of the first medical grade nanoclay called RENOVITE®. Several UKRI councils supported the underpinning research, spin-out founding and commercialisation. This includes BBSRC Follow-on Fund Pathfinder funding for market research and proof of concept studies, and MRC funding for 3D imaging systems at University of Southampton to view tissues and scaffolds at different scales.
Recently, Renovos was granted Breakthrough Device Designation by the US Food and Drug Administration for its RENOVITE® BMP-2 product. This nanoclay gel doesn’t leach BMP-2 and degrades as new bone forms at the target site, offering a safe method for localised directed tissue regeneration.
More pathways for progress
Since 2017, Renovos has raised further public and private sector funding for its innovative technology. This includes Innovate UK, Orthopaedic Research UK, and funding from healthcare accelerator ‘HS.’. BBSRC, EPSRC and MRC funding has also not halted:
- BBSRC funding, led by Professor Oreffo, that found it was possible to label skeletal stem cells with unique nanolabel tags to isolate and identify skeletal cell populations
- several Innovate UK grants, led by Dr Agnieszka Janeczek, that have accelerated the development of RENOVITE® for therapeutic use
- MRC, BBSRC and EPSRC funding that established the UK Regenerative Medicine Platform, made up of three interdisciplinary research Hubs (the Acellular/Smart Materials – 3D Architecture Hub is supporting Professor Oreffo’s and Dawson’s hydrogel and tissue engineering research)
- Future Leaders Fellowships funding for Dr Janeczek to use nanoclay gels in cell therapy
- MRC funding, led by Professor Dawson, for a UK-Japan collaboration to study how our immune system responds to nanoclay and attracts stem cells
Professor Oreffo says:
Among the challenges posed by our ageing population is the need for novel and cost-effective solutions to bone repair. Musculoskeletal disorders affect over 20 million people across the UK with an NHS cost of more than £5 billion. Interdisciplinary strategies harnessing skeletal stem cell-based therapies offer some of the most exciting and promising areas for bone disease treatment and bone regenerative medicine.
For over 20 years, I have been fortunate to receive direct grant support from the BBSRC to examine bone stem cells isolated from adult tissue. This includes bone marrow together with scaffolds from a range of materials to develop bone in the lab, plus being able to translate our research through to tangible patient benefits for real world problems.
Find out more
Read the 2021 REF case study, Therapeutic and commercial translation of skeletal stem cells for new approaches to orthopaedic treatment.
Visit the official Renovos website.