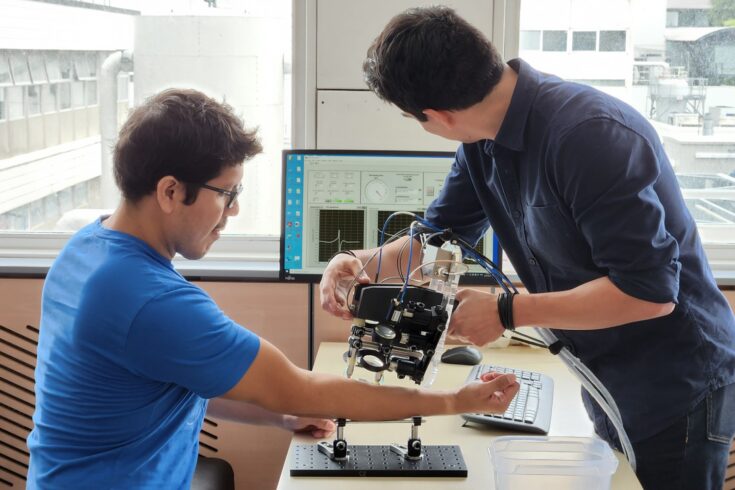
An innovative skin scanner aims to make surgery to remove skin cancers much faster, speeding up treatment, increasing patient throughput and saving the NHS money.
The ‘skinometer’ is the first-ever patient measurement device to harness light from the part of the spectrum where infrared and microwaves meet. It will enable surgeons to establish the exact extent of the cancer before surgery.
It has been developed by researchers at the University of Warwick, supported by the Engineering and Physical Sciences Research Council (EPSRC), part of UK Research and Innovation.
Improving on current practice
Current practice can require taking and testing multiple skin samples during the procedure. Using the device could, for example, mean a 3-hour surgical procedure to remove a skin cancer takes just half an hour to perform.
The skinometer has just started undergoing preliminary testing on patients at University Hospitals Coventry and Warwickshire (UHCW) NHS Trust and a handheld version has already been developed for easier, more mobile use.
Accelerating treatment times
The skinometer produces tiny pulses of light from the terahertz part of the spectrum, which strike the skin’s surface and bounce off.
The waveforms of the reflected light show how far the skin cancer has spread beneath the skin. Knowing this prior to surgery will mean the surgery can be completed faster and with better skin graft planning. The device is completely safe and causes no discomfort at all.
The skinometer is also designed to accurately indicate moisture levels in the skin and how the skin reacts to different moisturisers.
Effective sun creams
Extensive collection of such data from a wide range of people will aid development of more effective, skin-type-specific sun creams. The Warwick team are collaborating with speciality chemicals company Lubrizol to explore the possibilities.
Professor Emma MacPherson from Warwick’s Department of Physics who has led the research said:
Skin cancer rates have increased rapidly in the UK in recent decades, with over 16,000 new cases identified every year.
As well as helping prevention by aiding sunscreen development, the new skinometer will speed up the treatment pathway, achieving better outcomes, reducing patient stress and making more effective use of NHS resources.
It could potentially enter clinical use within 5 years and, beyond that timeframe, could eventually become a feature of GPs’ surgeries.
My vision is that ultimately the technology can also be extended to benefit detection of a variety of different cancers such as breast and colon cancers.
Faster, more effective treatments
Professor Dame Lynn Gladden, EPSRC Executive Chair said:
Engineering and physical sciences research plays a key role in developing new healthcare technologies that can help us live healthier for longer.
This new tool not only has the potential to improve sunscreens to protect us in the sun but can also detect how far skin cancers have spread under the skin, thereby enabling faster, more effective treatments.
Tailor-made treatment
Professor Joe Hardwicke, a skin cancer surgeon at UHCW, added:
This new technology may give us the ability to diagnose cancers in living tissue in real time and avoid the need for biopsy in the future for certain cancer types.
This will speed up diagnosis and could provide a tailor-made treatment for each patient.
Close collaboration
The ‘Terahertz Skinometer for Improved Cancer Prevention and Treatment’ research project began in March 2019 and is due to run until December 2022. It has received around £653,000 in EPSRC funding. Additional support has been provided by Cancer Research UK.
The research has involved close collaboration with Professor Joseph Hardwicke, a skin cancer surgeon at UCHW, Professor Vas Stavros of Warwick’s Department of Chemistry and Dr Christophe Corre from the Department of Life Sciences.
A new 5-year programme ‘Terabotics: Terahertz Robotics for Surgery and Medicine’, also supported by EPSRC, is investigating how robotics could be used to enable the skinometer to operate automatically and be extended to other cancers including colon cancer.